Healthcare claim denials challenge medical providers more than ever, making effective denials management in healthcare an essential part of medical claims management and overall healthcare revenue cycle performance. As payer rules and insurance requirements grow more complex, the denial rate continues to rise. These denials delay payments, increase administrative work, and reduce revenue. To protect their financial health, healthcare organizations must take a more strategic and proactive approach to managing claim denials.
Understanding Why Claims Get Denied

Insurance companies deny claims when providers submit missing or incorrect information, fail to verify eligibility, or don’t meet documentation or prior authorization requirements.
Even minor errors, like a wrong code or a misspelled name, can trigger a denial. Complex denials often result from changing payer rules or unclear communication between providers and insurers. These issues have become more common and financially damaging the Growing Impact of Denials.
Although denials have been a longstanding issue, they are now occurring more frequently and costing providers more. Staff members spend time and resources reviewing, correcting, and resubmitting claims. In many cases, providers don’t appeal denied claims, which causes permanent revenue loss.
These denials not only delay payments but also disrupt the entire healthcare denials management revenue cycle, especially when unresolved over time. Staff must shift time away from patient care to fix billing problems. Over time, unresolved denials weaken a provider’s cash flow and make daily operations more difficult.
These recurring issues highlight the need for automated claim denial management solutions that can flag and correct common errors before submission.
Issues such as lack of medical necessity or improper coding often result in clinical denials in healthcare, which are more complex and time-consuming to resolve.
Moving Beyond Reactive Denial Management

Many organizations traditionally respond to denials only after they happen. They may correct errors and resubmit claims, but this reactive approach wastes time and limits efficiency. A more effective approach focuses on preventing denials in the first place.
To prevent denials, providers must identify their root causes and fix them at the source. This process involves reviewing claim trends, tracking common rejection reasons, and refining workflows to prevent repeated mistakes.
Partnering with healthcare claim denial consulting services can also help in shifting from reactive corrections to proactive strategies.
The Role of Technology in Denial Prevention

Modern denial management tools help healthcare organizations control and reduce denials. These systems collect and analyze denial data to reveal patterns and problem areas. With these insights, billing teams can reduce errors and improve first-pass acceptance rates.
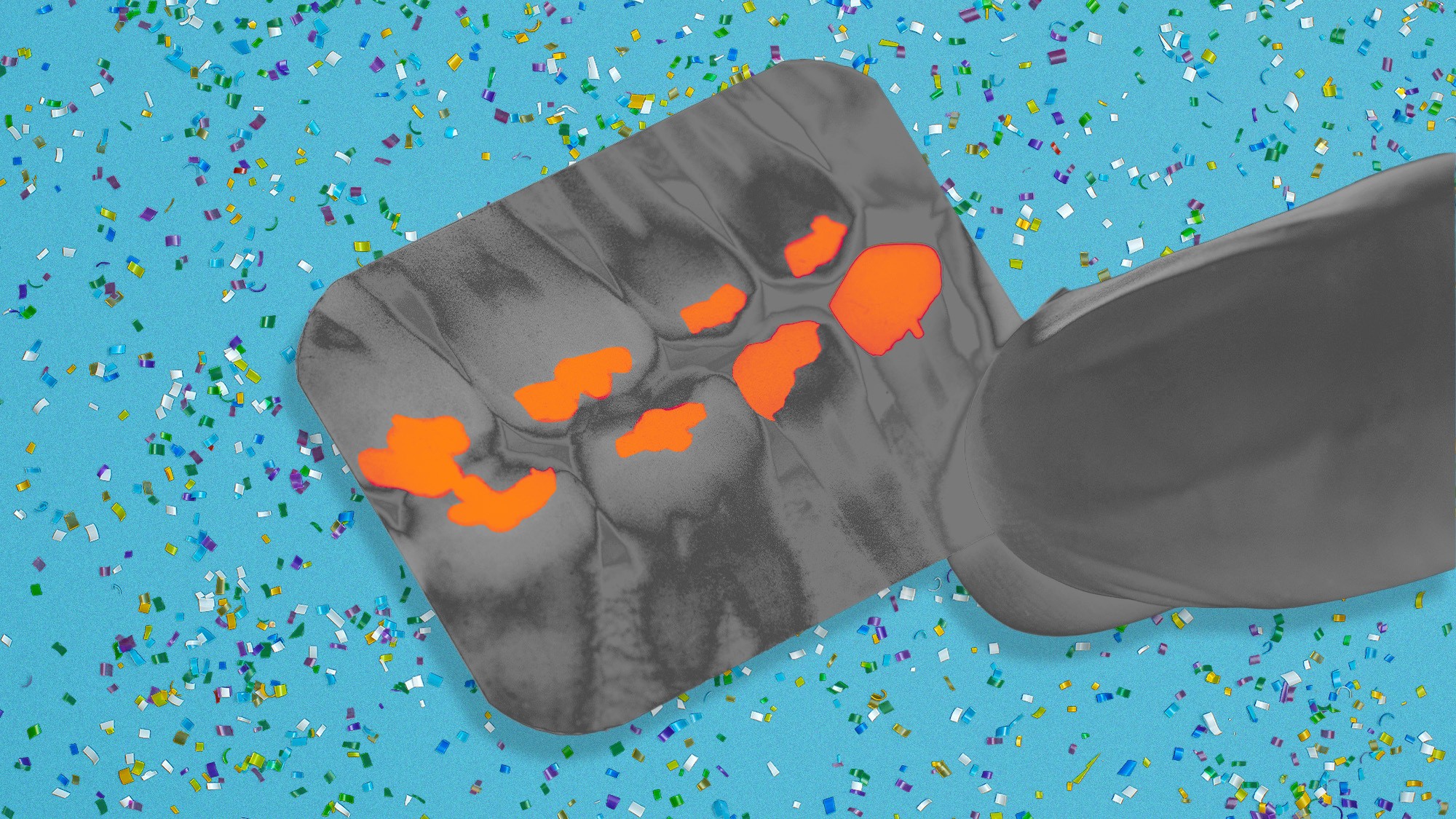
Healthcare analytics tools offer even more value. They analyze past claims to predict which ones may face denial. By flagging potential issues early, the system enables providers to correct claims before submission, thereby increasing their chances of having the claims approved.
Automation Improves Efficiency

As part of broader healthcare automation solutions, denial management tools are increasingly integrated with mobile medical claim management systems for healthcare, enabling real-time alerts and adjustments from anywhere.
Automation plays a significant role in efficient denial management in healthcare. Automated tools verify patient eligibility, check for prior authorizations, and review documentation before claim submission. These systems reduce human error and ensure claims meet payer requirements from the start.
For example, automated systems flag missing information or detect common coding errors in real-time. This feature helps staff correct claims before submission and avoid preventable denials. Automation also speeds up repetitive tasks, allowing staff to focus on more complex cases.
These automated systems also integrate well with medical billing and medical credentialing processes to ensure complete and accurate submissions.
Custom Denial Insight Platforms

Some providers opt for a custom denial insight platform instead of generic tools, and developers design these platforms to align with the provider’s payer mix, specialties, and workflow needs.
Custom platforms provide deeper visibility into denial causes and generate reports that help teams prioritize high-value claims. These tools also support more effective denial prevention strategies, such as updating documentation processes or improving training.
Tracking and Reporting Tools Matter

Effective claim denial management system software goes beyond listing denied claims. These tools generate clear, actionable reports that highlight trends by payer, procedure, and department, providing a comprehensive view of healthcare costs and expenses. With this information, teams can identify recurring problems and take corrective action.
Tracking tools also improve accountability. Billing teams can monitor their progress, measure improvement, and make data-driven decisions that will enhance the revenue cycle management solution.
Investing in healthcare denial management software enables real-time tracking, audit trails, and improved staff collaboration.
Consulting Services Provide Added Support

Healthcare providers often utilize healthcare claim denials management services and consulting experts. Consultants use their industry knowledge to identify issues within the current claims process.
They evaluate workflows, find gaps or inefficiencies, and recommend improvements. They also support the implementation of new tools and train staff to handle denials more effectively. These changes enable organizations to recover revenue more quickly.
Specialized medical claim denial management services help providers recover lost revenue by handling appeals and guiding system improvements to enhance efficiency.
Benefits of a Strategic Approach
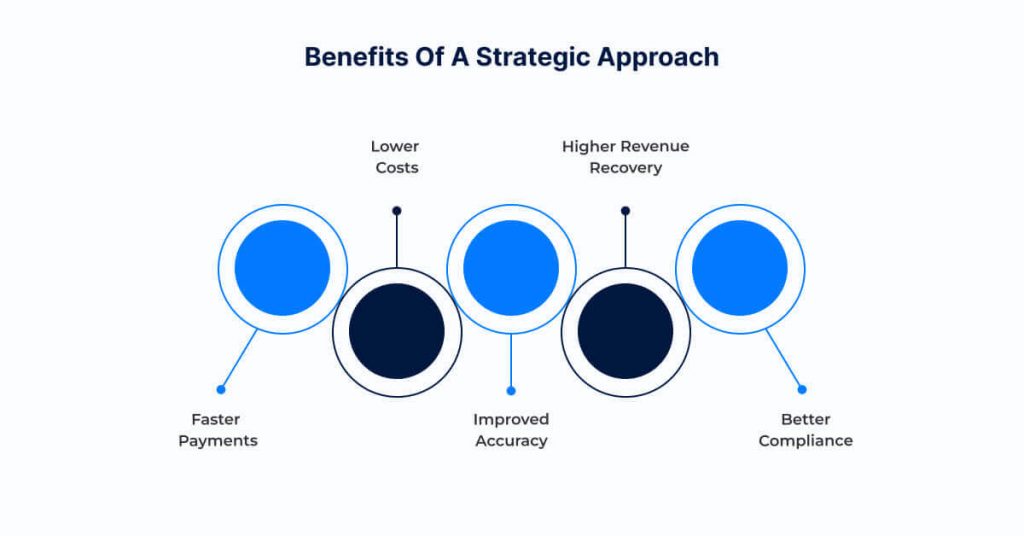
A proactive and strategic approach to denial management offers several key benefits:
- Faster Payments: Fewer denials allow providers to receive payments more quickly.
- Lower Costs: Automation and better processes reduce the time and labor needed to resolve denials.
- Improved Accuracy: Predictive tools and automated checks help providers catch errors early.
- Higher Revenue Recovery: By tracking and appealing denied claims, providers recover more lost revenue.
- Better Compliance: With improved workflows and documentation, providers keep up with payer rules.
- Stronger Forecasting: Leverage healthcare predictive analytics to identify at-risk claims and forecast potential denials.
Conclusion
Claim denial management is more than fixing billing errors; it’s essential to financial health. As payer rules change and denials increase, providers must shift from a reactive to a proactive approach.
Healthcare organizations that invest in denial management tools, healthcare analytics, automation, and predictive analytics for healthcare claim denials, along with expert support, can reduce claim errors, expedite payments, and safeguard their bottom line.
In today’s complex healthcare environment, those who effectively manage denials remain financially strong and deliver better care.
References
- https://www.healthjobsnationwide.com/blog/healthcare-denials-2025-hidden-reasons/
- https://akasa.com/blog/healthcare-claims-denials-are-at-an-all-time/
- https://gebbs.com/blog/strategic-denial-management-protect-healthcare-revenue-in-2025/
- https://helpsquad.com/claims-denial-management-in-2025/
The post The Ultimate Guide to Handling Healthcare Claim Denials Efficiently appeared first on Osplabs.