Introduction
Imagine a patient using a digital therapeutics app that tracks vital signs and collects self-reported questionnaires. The patient interacts with the app regularly, allowing for a comprehensive picture of their health journey to be built. However, clinicians need to manually enter the app data into the EHR. The struggle is real, the clinician’s time is lost and the focus on patient care is compromised. Well, these challenges need a quick yet simple solution- EMR/EHR system integration for health apps. Integrating mHealth solutions with EHRs ensures that patient data is directly stored in a centralized database without any manual intervention, enhancing both patient engagement and care coordination.
Today, several healthcare apps remain in this isolated space. Without integration, apps remain disconnected from clinical systems. This results in duplicate data entry, slow provider adoption, and inadequate care coordination. This makes EHR/EMR system integration for health apps a critical requirement to avoid silos and ensure care teams see the complete picture. What begins as a promising digital solution often ends up underutilized because it fails to integrate with the systems clinicians rely on every day.
When integration is done right, the picture changes. Integrating the EHR with healthcare applications will not only reduce administrative burdens but also facilitate seamless data exchange and enhance patient accessibility. Clinicians can now spend more time focusing on patient care rather than manually entering data into the EHR/EMR.
Health apps are typically innovative in their own right. However, integrating them with the EHR/EMR is a pressing need today. Let’s delve deeper to understand how to seamlessly implement EMR integration for healthcare apps.
Step-by-Step Implementation of EHR/EMR Integration with Healthcare Apps
Implementing EMR/EHR system integration for health apps requires a structured approach that aligns clinical workflows with technical execution. Here are some of the crucial steps.
Preparation & Discovery

Before connecting systems, it’s essential to review existing platforms, identify key stakeholders, and understand the existing workflows. Here’s what to focus on first.
- System and Interface Inventory
Start by reviewing all existing systems, including EHR/EMR platforms, app backends, device data feeds, third-party services, and data stores. Identify integration tools such as integration engines, API gateways, FHIR servers, message brokers, or iPaaS platforms. - Stakeholder Mapping
Identify stakeholders, including clinicians, IT staff, compliance officers, and the product team. Engage them early to align priorities, clarify roles, and secure buy-in for smooth execution. - Define Use Cases and Data Flows
Map which app features require access to specific clinical data. Define how data will be transferred between systems and ensure it aligns with real-world clinical workflows. This prevents redundancy and builds integration workflows tailored to the needs of providers. - Define Success Metrics
Set measurable criteria for success, such as data latency, accuracy, error rates, and provider adoption. These benchmarks track performance and guide future improvements.
Standards and Protocols

Choosing the right standards ensures reliable, scalable, and secure data exchange. Here’s how to select the protocols that matter.
- Standards Selection
Choose HL7 v2, HL7 v3, CDA, or FHIR depending on system compatibility and objectives. The chosen standard defines the foundation for consistent and reliable data exchange. - FHIR for Modern Apps
Adopt FHIR for its RESTful APIs, modular resources, and scalability. It simplifies integration for modern apps and supports future expansion. - SMART on FHIR
Implement SMART on FHIR to manage secure authorization and controlled access to clinical data. This ensures compliance and reduces risks of unauthorized access. - Legacy HL7
Use HL7 v2/v3 where needed, especially for workflows such as ADT feeds, orders, or messaging. These standards remain essential in many clinical environments. - XDS / Document Sharing
Apply XDS profiles for cross-system document exchange. This enables standardized retrieval and sharing of clinical documents across organizations.
APIs and Integration Tools
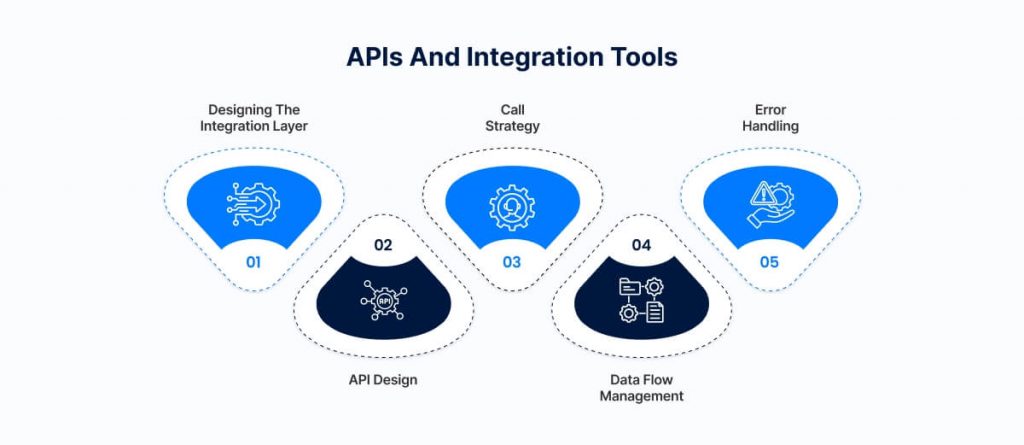
APIs and integration tools enable different systems, such as practice management solutions or RPM and EHRs, to communicate effectively. The following steps explain how to design this integration layer effectively.
- Designing the Integration Layer
Use integration tools or platforms to standardize communication between systems. This reduces complexity and makes long-term maintenance easier. Examples include integration engines, API gateways, and iPaaS platforms. - API Design
Define clear endpoints, resources, and versioning to ensure consistent communication. A well-designed API prevents miscommunication and ensures that app data is transmitted accurately to the EHR. - Call Strategy
Decide when to use synchronous calls for critical data and asynchronous calls for bulk or non-urgent data. This balances system responsiveness and reliability. - Data Flow Management
Utilize batching, pagination, and rate limits to effectively manage large volumes of data. This prevents system overload and ensures smooth operations. - Error Handling
Implement retry logic, idempotency(ensuring repeated operations don’t create duplicates), and failover strategies. These practices prevent duplicate records and ensure that workflows continue uninterrupted even in the event of errors.
Mapping and Transforming Data for the EHR
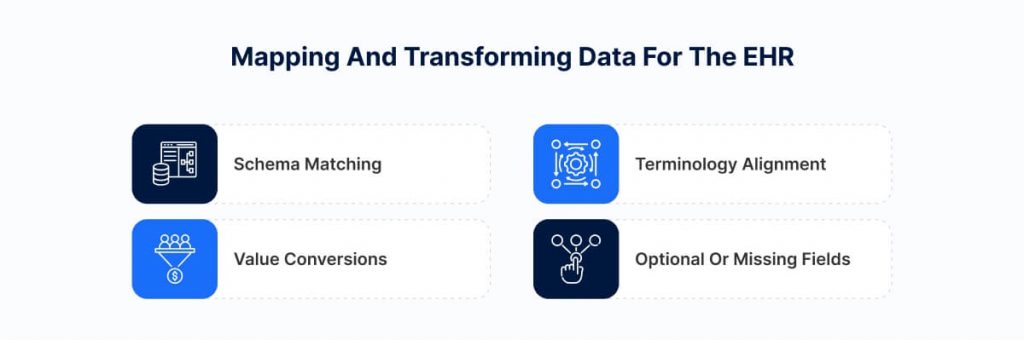
Mapping and transforming app data correctly ensures it is meaningful and actionable within the EHR. Consider the following best practices.
- Schema Matching
Map app fields to FHIR resources, such as Patient, Observation, and Condition. Proper mapping ensures accurate storage and interpretation in the EHR. - Terminology Alignment
Adopt standards such as SNOMED, LOINC, ICD, and RxNorm. This ensures consistent meaning and avoids misinterpretation across systems. - Value Conversions
Normalize units and validate incoming values. Reliable conversions improve data accuracy and clinical decision-making. - Optional or Missing Fields
Handle gaps using FHIR extensions when necessary. This prevents incomplete data from breaking workflows.
Securing Data and Access Management
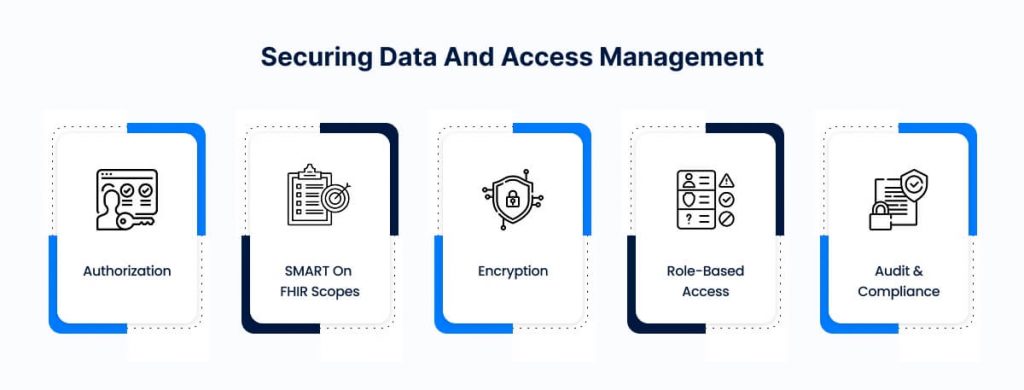
Securing sensitive health data depends on strong authentication, authorization, and encryption. The next section outlines the steps for implementing these safeguards.
- Authorization
Use OAuth 2.0 or OpenID Connect for secure authentication. These frameworks ensure only verified users gain access. - SMART on FHIR Scopes
Apply granular scopes to control access to specific resources. Fine-grained permissions reduce security risks. - Encryption
Encrypt data in transit with TLS and at rest with secure storage methods. This protects patient data from breaches. - Role-Based Access
Apply least-privilege access so users only see data required for their role. This maintains compliance and security. - Audit and Compliance
Maintain detailed logs, audit trails, and consent records to ensure accurate documentation. These safeguards enable traceability and ensure compliance with regulatory standards.
Testing and Validation
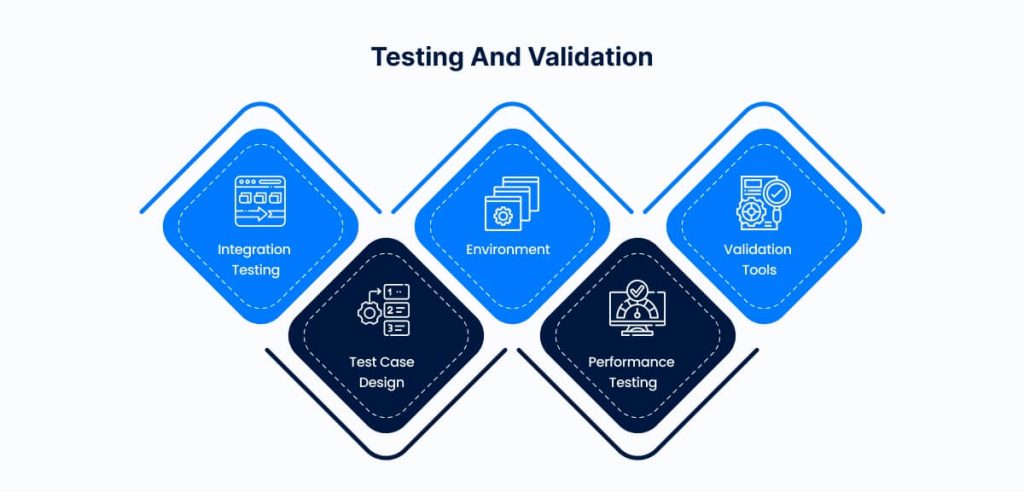
Testing confirms that all components can work together under real-world conditions. Here’s what to include in your validation process.
- Integration Testing
Conduct unit, component, and end-to-end tests to ensure systems work together as intended. Testing early minimizes costly errors. - Test Case Design
Include normal, edge, and failure scenarios. Comprehensive coverage ensures reliability under real-world conditions. - Environment
Use synthetic data and sandbox EHRs for safe testing. This protects live patient records from risk. - Performance Testing
Measure throughput, latency, and concurrency under load. Results confirm the system can scale without degrading performance. - Validation Tools
Leverage FHIR validators and schema checks to confirm compliance. This improves trust in the integration.
Pilot and Staged Deployment

Launching in a controlled environment allows safe adoption and early feedback. Here’s how to approach pilot deployment.
- Start Small
Launch with a limited set of users or features. A phased approach reduces risk and simplifies troubleshooting. - Monitor Performance
Track error rates, latency, and data accuracy during the pilot. Continuous monitoring ensures stability. - Collect Feedback
Engage clinicians and end-users for feedback on usability and workflows. Early input improves adoption. - Iterate
Refine mapping, workflows, and error handling based on pilot results. Iteration ensures readiness for broader rollout.
Full Rollout and Monitoring

Expanding to a full rollout ensures all users benefit while monitoring maintains system stability. Here’s what to focus on next.
- Expand Deployment
Roll out to the full user base after successful pilots have been conducted. A wider release ensures benefits reach all stakeholders. - Ongoing Monitoring
Utilize dashboards, alerts, and log reviews to promptly detect and resolve issues. Proactive monitoring supports system reliability. - Analytics
Track usage, latency, errors, and adoption trends to gain insights into your network’s performance. Analytics guide improvements and validate success. - Maintenance
Plan for upgrades, version changes, and schema extensions. Regular maintenance supports long-term sustainability.
A robust integration approach relies on healthcare cloud solutions and EHR data, providing secure, scalable access for remote teams.
The right integration specialists can seamlessly connect custom healthcare software development solutions or healthcare app development services to ensure that the application’s features align with clinical data standards and provider workflows. This structured approach supports secure authentication, data mapping, and compliance with regulations such as HIPAA.
Why This Process Matters

A structured integration process ensures interoperability, preserves data integrity, and builds clinician trust. Here’s why following these steps is critical-
- Ensures Interoperability and Scalability
A well-designed EMR/EHR integration enables seamless data exchange between health apps and clinical systems. Standardized workflows and integration tools decouple the app from specific vendors, support multiple EHRs, and enable future expansion. This approach ensures that the system grows reliably as new features, data types, or integrations are added. - Efficiency and Predictability
Following a structured integration process reduces guesswork and prevents errors that could require costly rework. Clearly defined phases, responsibilities, and success metrics create a predictable path, ensuring each step proceeds smoothly and systematically. - Data Integrity and Safety
Accurate data mapping, validation, and error-handling protocols prevent corruption, mismatches, and lost information. Maintaining the integrity of clinical data ensures that decisions are based on complete, trustworthy information. - Interoperability and Vendor Neutrality
Using standard protocols like FHIR, HL7, and CDA, combined with a middleware layer, decouples the app from EHR vendor-specific implementations. This enables the health app to work across multiple systems without requiring point-to-point customization. - Clinician Adoption and Trust
Reliable, automated data flow into the EHR reduces manual effort and increases clinician confidence in the app. When clinicians trust the system to provide accurate, actionable information, adoption rates improve, and integration delivers measurable value to care teams. - Scalability and Extensibility
A structured approach allows the integration to accommodate future organizational needs, such as additional app features, new clinical data types, or connections to more EHR systems. Scalable integration ensures the solution remains relevant and effective over time.
Challenges and Practical Solutions

- Partial or Inconsistent FHIR Implementation
Some EHRs support only a subset of FHIR resources, which limits their functionality. Use fallback mechanisms, such as HL7 messaging or custom APIs, to maintain reliable data exchange. - Terminology Mismatches and Local Codes
Differences in coding systems can result in data errors. Use mapping tables, integration tools, or translation services to standardize data across systems. - Performance and Latency Under Load
High volumes of data or concurrent users can cause delays in system response. Utilize batching, caching, asynchronous queues, and backpressure mechanisms (techniques for managing system overload) to maintain smooth performance. - Error Spikes and Exceptions
Unexpected failures can disrupt clinical workflows. Implement retry logic, dead-letter queues, and alerting systems to quickly detect and resolve errors. - Versioning and Schema Changes
API updates or schema changes may break integrations. Design versioned APIs and compatibility layers to ensure backward compatibility and minimize disruption. - Stakeholder Resistance and Workflow Disruption
Clinicians and staff may resist new tools or processes. Engage stakeholders early, provide simulations and training, and integrate solutions seamlessly into existing workflows to encourage adoption. - Data Privacy and Patient Consent
Sensitive patient information must remain secure. Implement granular consent flows, data segmentation, and encryption to comply with regulatory requirements and maintain trust. - Vendor Cooperation and Proprietary APIs
Some EHR vendors restrict API access. Utilize middleware adapters, negotiation, or certified integration engines to facilitate data flow while adhering to proprietary constraints.
Benefits of Successful Integration
- For Healthcare Providers and Institutions
When integration is done right, EHR-connected apps not only reduce administrative burdens but also facilitate seamless data exchange. Leveraging healthcare automation solutions, providers can minimize duplicate data entry, streamline workflows, and devote more attention to patient care. - For IT Teams
A unified integration layer reduces the need for multiple point-to-point connections, simplifying system management and maintenance. Modular architecture enables faster onboarding of new features and easier scaling across multiple EHRs or healthcare systems. - For Patients and App Users
Seamless data flow into medical records ensures a consistent user experience. Patients benefit from better continuity of care, as health apps become a trusted component of the clinical ecosystem. Accurate, real-time data also supports more personalized and timely care interventions. - Business Value for the Health App
Successful integration enhances market differentiation and adoption within care networks. It enables data-driven insights, supports advanced app functionality, and strengthens the app’s credibility as a reliable tool in clinical workflows.
Conclusion
EMR/EHR system integration for health apps unlocks a health app’s full clinical potential, enabling seamless data flow and reducing vendor-specific complexity. Selecting the right integration approach ensures that app data aligns with clinical workflows and supports reliable decision-making. Healthcare organizations and app developers should first assess readiness, initiate a pilot deployment, and collaborate with experienced integration partners to ensure a smooth implementation. A structured approach enables organizations to achieve interoperability, allowing them to integrate their health app with EHR systems and unlock their full clinical potential.
OSP’s expertise ensures smooth data exchange, optimized workflows, and measurable value for providers, IT teams, and patients. Leveraging professional guidance ensures that integration delivers measurable value to clinicians, IT teams, patients, and the overall healthcare ecosystem.
References
- https://docs.smarthealthit.org/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9750793/
- https://topflightapps.com/ideas/how-integrate-health-app-with-epic-ehr-emr/
- https://www.ibm.com/think/insights/hl7-fhir-integration
- https://www.thinkitive.com/blog/hl7-ehr-integration-guide/
- https://www.healthit.gov/playbook/electronic-health-records/
- https://www.techmagic.co/blog/healthcare-integration
The post How to Implement EHR/EMR Integration with Your Health App System appeared first on Osplabs.










