Written by Joanne Byron, BS, LPN, CCA, CHA, CHCO, CHBS, CHCM, CIFHA, CMDP, OHCC, ICDCT-CM/PCS
This article emphasizes the need of healthcare institutions to focus on building a culture of safety through Root Cause Analysis (RCA) to Manage Clinical Risk is an important management tool. Read Part 1: Building a Culture of Patient Safety Starts with Reducing Staff Burnout posted December 3, 2024 and Part 2: An Approach to Reduce Patient and Workforce Harm.
Introduction
Keeping patients safe requires an organizational culture of safety based on the commitment from Directors and C-Suite Executives. Creating a patient safety environment includes complex interventions that involve the need for variations in individual work routines and healing processes as well as behavioral changes to be made on the part of the team or the individual for maximum acceptance from others.
Patient safety is a framework of organized activities that creates cultures, processes, procedures, behaviors, technologies and environments in health care that consistently and sustainably lower risks, reduce the occurrence of avoidable harm, make error less likely and reduce its impact when it does occur.
Every point in the process of care-giving contains a certain degree of inherent unsafety.
Clear policies, organizational leadership capacity, data to drive safety improvements, skilled health care professionals and effective involvement of patients and families in the care process, are all needed to ensure sustainable and significant improvements in the safety of health care.
Root Cause Analysis & Patient Safety
Most healthcare organizations use RCA as a tool to find out what happened, why it happened, and how to prevent it from happening again. The process is a tool for identifying prevention strategies. It is a process that is part of the effort to build a culture of safety and move beyond the culture of blame.
In a Root Cause Analysis Program, basic and contributing causes are discovered in a process similar to diagnosis of disease – with the goal always in mind of preventing recurrence. The following information breaks this complex process down into basic bullet points and serves as an introduction to this topic only.
What the RCA process is:
- An inter-disciplinary, involving experts from the frontline services;
- Successful when you involve those who are the most familiar with the situation;
- A process which requires diligence – continually digging deeper by asking why, why, why at each level of cause and effect;
- A process that requires your organization to identify changes that need to be made to systems; and
- A process that must be performed with objectivity and as impartial as possible.
What RCA Should Encompass:
- Determination of:
- human and other factors;
- Related processes and systems
- potential improvement in processes or systems
- Analysis of underlying cause and effect systems through a series of why questions
- Identification of risks and their potential contributions
For Your Program to be Credible, an RCA must:
- Adopt a top-down approach
- Include participation by the leadership of the organization and those most closely involved in the processes and systems
- Be internally consistent
- Include consideration of relevant literature
The Safety Assessment Code (SAC)
The Safety Assessment Code (SAC) can be used to determine whether or not an RCA must be conducted, based on the severity of a specific incident and its probability of occurrence. It is a method for determining whether any further definitive action is required concerning a particular incident based on the severity of the incident and its probability of occurrence.
A “SAC score” is also of value for incidents that did not result in an adverse event but may also lead to an RCA; i.e., a close call. Close calls occur far more frequently than adverse events and can provide an exceptional opportunity for learning. Close calls afford the chance to develop preventive strategies and actions before a patient may be harmed.
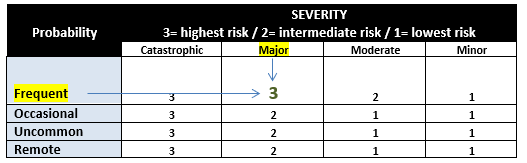
The SAC Matrix is a tool for combining severity and probability. While either the severity or probability of occurrence could be determined first, it is usually more productive to assess the severity first.
When you pair a severity category with a probability category for either an actual event or close call, you will get a ranked matrix score. These ranks, or Safety Assessment Codes (SAC), can then be used for doing comparative analysis. There are various SAC matrix tables available, the one below uses 3 severity and 4 probability categories.
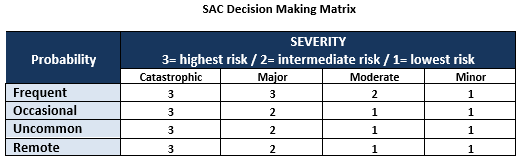
While either the severity or probability of occurrence could be determined first, it is usually more productive to assess the severity first. This is true since until one has determined the severity of an incident it would be difficult if not impossible to assess an appropriate probability level. Intersect the 2 categories to determine the SAC score. For example, if the probability of the adverse event happening if frequent and it is determined by the team that it ranks a severity of “3”, then result would be mapped in the table below.
3 = highest risk
2 = intermediate risk
1 = lowest risk
The utility of the SAC is at the start of the process so that resources are applied where they have the greatest opportunity to improve the level of safety from a systems perspective.
Root Cause Analysis (RCA) Versus Healthcare Failure Mode & Effects Analysis (HFMEA )
)
HFMEA is a technique that is usually performed on a system to assess and prioritize the risks associated with that system in the hopes of reducing the risks through re-design as a proactive measure. Both Root Cause Analysis (RCA) and Healthcare Failure Mode and Effects Analysis (HFMEA
is a technique that is usually performed on a system to assess and prioritize the risks associated with that system in the hopes of reducing the risks through re-design as a proactive measure. Both Root Cause Analysis (RCA) and Healthcare Failure Mode and Effects Analysis (HFMEA ) possess the following elements:
) possess the following elements:
- Both are non-statistical methods of analysis
- The goal of both is to reduce patient harm
- Both involve identifying conditions that lead to harm
- Both are team activities
Many people confuse these terms and believe that they compete against each other when in fact neither of these two techniques can accomplish what the other can. They are complementary to each other. A “root cause” is the most fundamental reason for a failure or situation where performance does not meet expectations.
- Root cause analysis is routinely conducted reactively – to probe the reason for a poor or unexpected outcome or failure which has already occurred.
- A recent use of root cause is to conduct such analysis as part of a proactive risk reduction effort using Healthcare Failure Mode and Effects Analysis (HFMEA
 ).
).
The table below provides a side-by-side comparison of these two analytical tools used in health care.
|
RCA Required by Joint Commission after a sentinel event |
HFMEA Proactive approach to prevent system-related failures |
|
Similarities
|
|
|
Differences RCA HFMEA |
|
|
Reactive |
Proactive |
|
Focuses on an event |
Focuses on entire process |
|
Hindsight bias |
Unbiased |
|
Fear, resistance |
Openness |
|
Asks: “Why?” |
Asks: “What if?” |
Summary
Organizational culture refers to the shared beliefs, values, and behaviors within a healthcare organization. A lack of emphasis on patient safety in organizational culture can hinder initiatives that aim to ensure patient safety. It may manifest itself as a lack of commitment, inadequate support, or insufficient prioritization of safety measures by the hospital’s leadership and staff. This can result in a higher likelihood of medical errors and adverse events occurring. A weak organizational culture can also discourage staff from reporting incidents or speaking out about potential safety concerns further compromising patient safety.
Building a culture of safety starts with educating your Board of Directors, a C-Suite Executives. The Compliance Department should oversee internal audits that not only include typical compliance risks related to fraud, waste and abuse, but measuring compliance to safety standards as well. Producing reports to present to high-level executives can help support the budget needed to mitigate patient risk of an adverse event.
To learn more about RCA, I recommend registering for the Certified Healthcare Auditor online certification training program which includes not only auditing, but using RCA for corrective action after the audit. To learn more about training as a healthcare Compliance Officer, I highly recommend the online Corporate Compliance certification program.
About the Author and AIHC
The author, Joanne Byron, shares her clinical, consulting, auditing and educational experience by serving as the Board Chair and overseeing the AIHC Volunteer Education Committee. She is also a volunteer hospice nurse, hospice hands-on-care volunteer and End of Life Doula.
The American Institute of Healthcare Compliance (AIHCR) is a non-profit healthcare training organization and a licensing/certification partner with CMS. Please visit our online store listing current training and certification offerings.
Copyright © 2024 American Institute of Healthcare Compliance All Rights Reserved
The post Culture of Safety is based on Prevention, not Punishment appeared first on American Institute of Healthcare Compliance.