This article is a part of your HHCN+ Membership
The Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey is a vital tool for measuring home health patient experiences. However, these surveys are often complex and can be unreliable feedback methods because of low patient response rates.
While home health providers, especially smaller organizations, may struggle to implement and leverage CAHPS data, survey results play a crucial role in informing consumers, supporting quality improvement efforts, and spurring value-based purchasing initiatives by organizations such as the Centers for Medicare and Medicaid Services (CMS).
“CAHPS surveys provide valuable insights into how well we’re meeting [patient] expectations,” Erin Volbeda, vice president of marketing and communications at Enhabit, told Home Health Care News. “We use this feedback not only to drive improvements but also to recognize and celebrate our clinicians when patient insights highlight exceptional care. It’s a meaningful way to reinforce our culture of compassion and excellence.”
Dallas-based Enhabit currently operates 249 home health locations and 114 hospice locations across 34 states.
CAHPS surveys, which are supported by the Agency for Healthcare Research and Quality (AHRQ), assess key elements of health care quality, including communication between patients and providers, ease of access, customer service from health plans and coordination among providers.
Providers told Home Health Care News they use CAHPS data to improve care, support patient decision-making, promote accountability and facilitate performance-based payments for high-quality services.
CMS regards CAHPS as the gold standard for measuring the quality of patient experience and uses the data for its value-based programs, impacting provider payments
The shift to paying providers within a value-based care system, rather than a fee-for-service model, emphasizes the importance of assessing patient experiences with their health care providers.
CAHPS surveys also help hold providers accountable for poor care. Patient complaints can identify concerns with a facility or provider. When a provider consistently scores low on surveys, CMS is notified of these issues and may decide to investigate.
Translating data into meaningful results
Enhabit Home Health and Hospice uses these survey responses in its Quality Assurance and Performance Improvement (QAPI) process to identify opportunities for enhancing care delivery, according to Erin Volbeda, vice president of marketing and communications.
“These insights help guide targeted education for our clinical teams and reinforce best practices that align with patient expectations and experiences,” she told Home Health Care News.
Similarly, CenterWell Home Health uses the comments from the surveys, as well as overall scores, to develop action items or customer service initiatives that are incorporated into its QAPI program, according to Chief Clinical Officer Sherri Rains.
“The comments and performance metrics are reviewed monthly and action items are updated and implemented at least quarterly based on survey findings and trends,” she said. “Each patient’s experience and feedback is important to us, so educating patients about the potential to receive a survey and expressing our appreciation if they take the time to complete the survey is paramount to a successful CAHPS program.”
CenterWell is Humana’s provider services arm, which includes home health, pharmacy and primary care.
AHRQ provides resources such as the CAHPS database and the Ambulatory Care Improvement Guide to help organizations use results for quality improvement, while new surveys, supplemental item sets and patient narrative tools reflect the program’s ongoing innovation, according to an AHRQ spokesperson.
When determining how to translate CAHPS survey results into meaningful quality improvements, the most challenging aspect can often be knowing where to start. Providers need to identify which questions from the survey most affect their score, according to Katie Wehri, vice president of regulatory affairs, quality and compliance at the National Alliance for Care at Home (the Alliance).
“With the workforce and operational challenges agencies are facing, they must be efficient and effective in their work, so identifying and focusing on the areas that have the greatest impact on their score will produce the best results,” Wehri told HHCN.
To identify the most influential questions, Wehri suggested that providers ask their survey vendors for the correlation coefficients of the questions. This indicates the strength of the relationship between each question’s top-box score and the agency’s overall rating. They can also carefully review any questions that are inversely related to their score, although this may require a detailed analysis of the composite questions linked to the performance measure.
Once the focus areas are identified, agencies can develop an improvement plan.
“This process must involve the team, and it’s important to keep that goal top of mind once it’s defined and maintained,” Wheri said. “Ongoing communication about progress toward the goal and maintaining it after achievement are essential for long-term success.”
Challenges
Despite the value of these surveys, researchers at RTI International identified challenges in conducting and sharing the results.
One common challenge is low response rates. Response rates are often used as an indicator of how well the data represent the population. Higher response rates enhance the validity of survey results, increase the likelihood that findings can be applied to the target group, and reduce the risk of nonresponse bias, according to RTI. Overall, slipping response rates have been a concern for survey researchers for a few decades, a sentiment shared by CAHPS survey users, stakeholders, sponsors, clinicians and accreditation organizations.
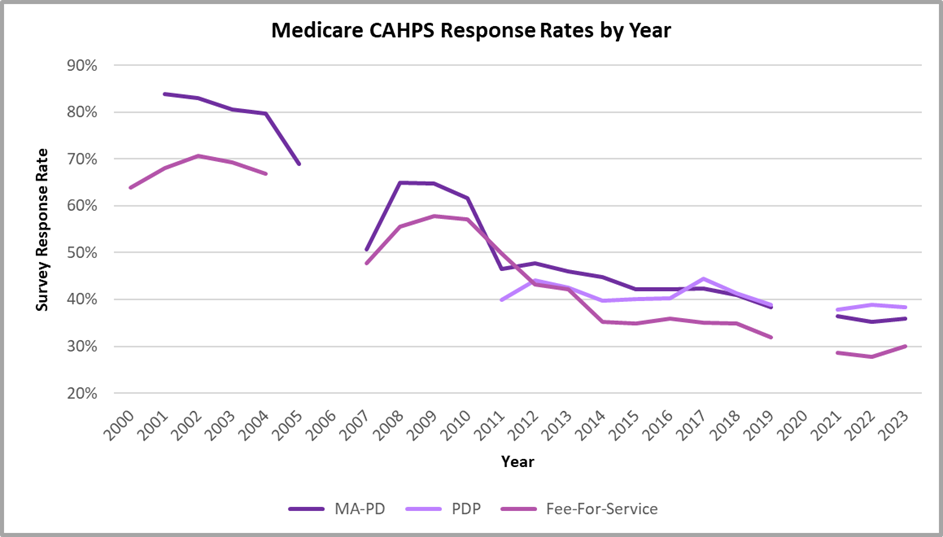 CMS data | CC0 CMS data | CC0
CMS data | CC0 CMS data | CC0“Providers using CAHPS surveys often encounter challenges, including limited detail from standardized questions, delays in receiving results, difficulty interpreting data and resource constraints – particularly for smaller organizations,” a spokesperson from AHRQ told HHCN. “Yet despite these barriers, CAHPS surveys remain vital. They provide a consistent, standardized way to capture what matters most to patients, identify opportunities for improvement, and complement other measures such as Patient-Reported Outcome Measures to give a fuller picture of care quality.”
However, as response rates continue to decline, the cost for home health providers of obtaining completed surveys from patients increases. Sample size is a significant factor influencing survey costs for mail and telephone methods, and the decreasing response rates demand ever-larger sample sizes.
RTI researchers noted that it might be possible to obtain accurate estimates without increasing sample sizes by using prior information to reduce variance.
RTI conducted preliminary research to measure the change in key estimates between completed mail surveys from the full mail protocol, a multi-step standardized process designed to maximize survey response rates and data quality, and those from only the first month of fielding. The forecast for the national and larger regions was nearly identical when comparing the first month only to the full mail protocol. It was concluded that providers with larger sample sizes, under the current methods, could reduce their sample sizes without sacrificing precision.
Researchers noted that incorporating new measures into these surveys can be challenging. However, surveys must remain relevant by including new questions that focus on the aspects of care most important to patients and providers at present.
Any new questions should follow the CAHPS measurement science principles of clarity and accuracy, focusing on whether respondents observed providers displaying specific behaviors, without allowing expectations or personal quirks to influence their answers. However, adding new questions often makes the surveys longer, which can discourage people from completing them, according to researchers.
AHRQ has begun examining how survey length affects the effectiveness and cost of data collection, as well as its relationship to overall response rates. However, research findings on the relationship between survey length and response rates have shown mixed results.
Recently, changes were made to the CAHPS hospice survey to reduce the number of questions, update the wording and offer a web-based option for caregiver response, according to Wehri.
“While these are welcome changes that the hospice community has been requesting, time will tell if they succeed in meeting one of CMS’ goals – improving survey response rates,” Wehri said. “Perhaps the biggest challenge in boosting CAHPS scores and quality of care is the time it takes to see results from the efforts. This makes it especially important to gather feedback outside of the survey, such as through real-time patient surveys.”
Agencies seeking this real-time information from patients must still adhere to the CMS CAHPS guidelines regarding communications that could improperly influence the CAHPS survey, Wehri said. However, within the parameters, there are options for feedback that allow for more timely action in addressing potential misunderstandings or problems.
Opportunities for improvement
Some CMS programs are addressing the problem of low response rates by distributing educational materials, such as flyers or posters, to patients through their providers. These materials explain the basic purpose and legitimacy of the survey. An endorsement from a trusted provider conveys that this is a legitimate survey, which can be meaningful in a patient’s decision whether to complete it. Home health agencies with higher employee engagement are more likely to experience high patient and caregiver satisfaction scores, according to a report from BerryDunn, a tax, advisory and consulting firm and sponsored by Strategic Healthcare Programs and the Alliance.
“We proactively educate patients and their caregivers about the purpose and importance of the CAHPS survey,” Volbeda said. “By emphasizing how their feedback directly informs our quality improvement efforts, we encourage participation and reinforce our commitment to delivering exceptional care.”
Rains emphasized the importance of communication and care coordination as key components of CAHPS survey questions. To receive positive results on CAHPS surveys, these two clinical skills must be well executed, she said.
“To do that, we educate our clinical associates on the evidence-based communication strategies of ‘motivation interviewing’ and ‘teach-back method,’” she noted. “These established strategies are about meeting patients where they are and gathering input from them in a way that’s meaningful to them. We listen and we act upon what they’re saying in guiding our care coordination. This drives better engagement, participation and patient satisfaction.”
In addition, Rains said CenterWell continually updates and enhances its case conference processes and documentation of care coordination in the medical record.
The number of surveys a person receives has also been identified as a contributing factor to declining response rates. In CAHPS surveys of the home health, outpatient surgery and dialysis settings, CMS specifies that a person can be sampled no more than twice a year.
CMS currently allows home health care CAHPS surveys to be administered electronically, primarily through mixed-mode approaches with mail or telephone, with data collected by CMS-approved survey vendors. After investigation, the agency acknowledged that electronic options provide patients more choices and can improve response rates and data collection.
However, for providers like Enhabit, even online surveys can pose challenges.
“A significant challenge is ensuring survey accessibility for patients with cognitive or functional limitations, or those residing in assisted living facilities where survey completion may be more difficult,” Volbeda said. “Communication and care coordination are important drivers of patient experience.”
The post Making CAHPS Surveys Work: Home Health Providers’ Strategies appeared first on Home Health Care News.